January ADCES Blog Post – ADA 2023 Standards of Care: Changes to LDL Recommendations
Greetings Pharmacy COI Members – January marks a new year and a new set of guidelines from the American Diabetes Association. For the first blog post of the year, I wanted to highlight some notable changes to the LDL/statin recommendations found in Section 10: Cardiovascular Disease and Risk Management https://doi.org/10.2337/dc23-S010
|
Standard Recommendation
|
ADA 2022
|
ADA 2023
|
|
Primary Prevention
|
10.19 For patients with diabetes aged 40–75 years without atherosclerotic cardiovascular disease, use moderate-intensity statin therapy in addition to lifestyle therapy. A
|
10.18 For people with diabetes aged 40–75 years without atherosclerotic cardiovascular disease, use moderate-intensity statin therapy in addition to lifestyle therapy. A (no change)
|
|
10.21 In patients with diabetes at higher risk, especially those with multiple atherosclerotic cardiovascular disease risk factors or aged 50–70 years, it is reasonable to use high-intensity statin therapy. B
|
10.20 For people with diabetes aged 40–75 at higher cardiovascular risk, including those with one or more atherosclerotic cardiovascular disease risk factors, it is recommended to use high-intensity statin therapy to reduce LDL cholesterol by ≥50% of baseline and to target an LDL cholesterol goal of <70 mg/dL. B
|
|
10.22 In adults with diabetes and 10-year atherosclerotic cardiovascular disease risk of 20% or higher, it may be reasonable to add ezetimibe to maximally tolerated statin therapy to reduce LDL cholesterol levels by 50% or more. C
|
10.21 For people with diabetes aged 40–75 years at higher cardiovascular risk, especially those with multiple atherosclerotic cardiovascular disease risk factors and an LDL cholesterol ≥70 mg/dL, it may be reasonable to add ezetimibe or a PCSK9 inhibitor to maximum tolerated statin therapy. C
|
|
Secondary prevention
|
10.24 For patients with diabetes and atherosclerotic cardiovascular disease considered very high risk using specific criteria, if LDL cholesterol is ≥70 mg/dL on maximally tolerated statin dose, consider adding additional LDL-lowering therapy (such as ezetimibe or PCSK9 inhibitor). A
|
10.26 For people with diabetes and atherosclerotic cardiovascular disease, treatment with high-intensity statin therapy is recommended to target an LDL cholesterol reduction of ≥50% from baseline and an LDL cholesterol goal of <55 mg/dL. Addition of ezetimibe or a PCSK9 inhibitor with proven benefit in this population is recommended if this goal is not achieved on maximum tolerated statin therapy. B
|
The 2023 ADA Standards of Care has some notable changes to recommendations around LDL goals – see highlight changes in the table above which compares recommendations from the 2022 SOC to the 2023 SOC. Given the stricter LDL goals, we as pharmacists, may see an increase in non-statin therapies Rx at the pharmacy or those of us with CDTM may find ourselves starting these agents more so than previously to reduce CV risks. So, let’s review dosing information for ezetimibe and PCSK9i along with trial data to support use of these agents.
Zetia (Ezetimibe) 10 mg once daily
Mechanism – targets the Niemann–Pick C1–like 1 (NPC1L1) protein, thereby reducing absorption of cholesterol from the intestine. When added to statins, ezetimibe reduces LDL cholesterol levels by an additional 23-24%, on average.
IMPROVE-IT Trial (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) N Engl J Med 2015; 372:2387-2397 DOI: 10.1056/NEJMoa1410489
18,144 patients following a recent ACS event were randomized to receive simvastatin + ezetimibe or simvastatin + placebo. Baseline LDL in both groups was 94 mg/dL. Primary efficacy endpoint was time to death from CVD, major coronary event, or non-fatal stroke. The median time weighted average LDL was 54 mg/dL in the simvastatin-ezetimibe group vs 70 mg/dL in the simvastatin-placebo group. The Kaplan–Meier event rate for the primary end point at 7 years was 32.7% in the simvastatin–ezetimibe group, as compared with 34.7% in the simvastatin-monotherapy group (absolute risk difference, 2.0 percentage points; hazard ratio, 0.936; 95% confidence interval, 0.89 to 0.99; P=0.016). NNT =50
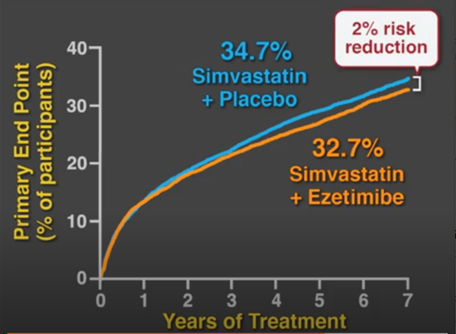
Conclusion – when added to statin therapy following an ACS event, ezetimibe reduced LDL and improved cardiovascular outcomes.
PCSK9i Mechanism: Proprotein convertase subtilisin/kexin type 9 (PCSK9) is an enzyme that binds to low-density lipoprotein receptors (LDL receptors), which stops LDL being removed from the blood, leading to an increase in blood levels of LDL. The PCSK9 inhibitor blocks the PCSK9 enzyme, resulting in more LDL receptors available to remove LDL from the blood, which produces in a decrease in LDL blood levels.
Repatha (evolocumab)
- 140mg SC every 2 weeks OR
- 420mg monthly

FOURIER Trial (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) N Engl J Med 2017; 376:1713-1722 DOI: 10.1056/NEJMoa1615664
which enrolled 27,564 individuals with prior ASCVD on moderate and high intensity statin therapy who still had LDL >70 mg/dL who were randomized to evolocumab vs placebo. Dosing of evolocumab was every 2 weeks or monthly based on patient preference. Evolocumab reduced LDL by 59% from median LDL of 92 mg/dL to 30 mg/dL in the treatment arm over 12 weeks. By 48 weeks, 87% of participants in the evolocumab group reached LDL goals of <70 mg/dL. During the 2.2-year follow-up the composite outcome of CV death, MI, stroke, hospitalization for angina, or revascularization occurred in 11.3% of placebo patients vs 9.8% of evolocumab participants, representing a 15% relative risk reduction (P<0.001) Importantly, similar benefits were seen in a pre-specified subgroup analysis of people with diabetes (11,031 patients or 40% of people enrolled).
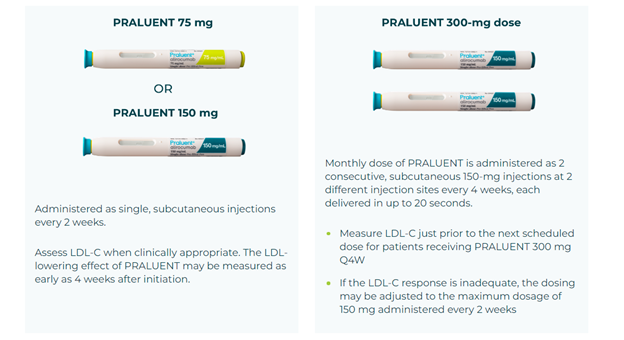
Praluent (alirocumab)
Starting dose is 75mg SC every 2 weeks or 300mg every 4 week
If LDL response is inadequate, can increase to 150mg every 2 weeks
ODYSSEY OUTCOMES Trial Schwartz GG, et al; ODYSSEY OUTCOMES Committees and Investigators. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med. 2018 Nov 29;379(22):2097-2107. doi: 10.1056/NEJMoa1801174.
(Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During the Treatment of Alirocumab) enrolled 18,924 patients (28.8% with diabetes) with recent ACS on maximally tolerated statin therapy were randomized to alirocumab or placebo given every 2 weeks. Alirocumab was titrated from 75 to 150mg if needed to target LDL between 25-50 mg/dL. Primary endpoints included death from CHD, nonfatal MI, fatal or nonfatal stroke, or unstable angina requiring hospitalization. Over a median follow-up of 2.8 years a composite primary endpoint occurred in 903 patients (9.5%) in the alirocumab group and in 1,052 patients (11.1%) in the placebo group (HR 0.85 [95% CI 0.78-0.93}; P<0.001). In the intention-to-treat analysis, mean LDL-C levels were 92 mg/dL at baseline. At month 48, they were reduced to 66 mg/dL with PRALUENT vs 103 mg/dL with placebo
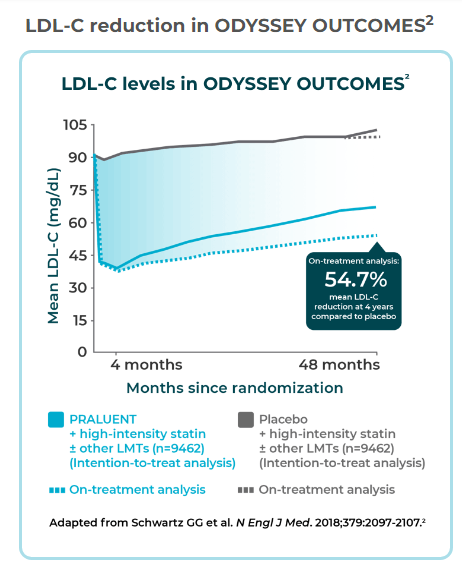
Conclusion: Both available PCSK9i have indications for use in patients with established CVD on maximally tolerated statin therapy. In clinical trials, both evolocumab and alirocumab lowered LDL and improved CV Outcomes. It is recommended to check LDL-C levels no sooner than 4 weeks after initiating a PCSK9i.
Impact on PharmD/CDCES:
- Educating persons with diabetes on the macrovascular complications of living with diabetes
- Educating patients on the benefits of medications to lower CV Risk such as statins, ezetimibe, and PCSK9i
- Educating patients on how to inject PCSK9i and use pens along with counseling on appropriate storage, disposal, and how to handle missed doses
- Assessing current medication regimens, including appropriateness of statin intensity and LDL target (<70 vs <55) and if meeting these goals
- Escalating therapy when LDL goals are not met
How will you be evaluating your patients for these changes?